Dads also tend to prefer soft structured carriers over wraps and slings because they feel a bit manliermore like wearing. Read about baby wraps vs.
 The Best Baby Carriers For Newborns And Toddlers In 2020
The Best Baby Carriers For Newborns And Toddlers In 2020
And when it gets dirty you can just toss it in your washing machine for easy cleaning.

Best soft structured baby carrier. It is the most basic model out of the ERGO range. Parents love soft structured carriers because they go on fast theyre easy to adjust and theyre more comfortable than wraps or slings for longer wears with heavier babies. Frameless soft-structured carriers vs.
LILLEBaby Complete All Seasons Baby Carrier. Extended torso removable sleeping hood and zippered storage pocket are some of the useful extras you can expect with this great carrier. The Free-to-Grow is easy to clean on the go and in your washer and dryer.
Why We Love It. The Baby Tula cotton canvas baby carrier has a huge devoted mom following for good reason. For more safety information check out this post.
See Now Add To Amazon Registry. They are all based around having a soft padded structure that. CLICK TO CHECK CURRENT PRICE.
This is a great soft-structured baby carrier with tons of features good looks and high versatility. Parents on a budget love this Infantino carrier from birth it works for babies as little as 8 pounds up until baby reaches 32 pounds in her toddler years. Best Affordable Soft-Structured Baby Carrier Infantino Flip 4-in-1 Convertible Carrier.
With six positions including front back and hip Plus a few more you and your little one have a lot of options. The LILLEBaby series is relatively new to the baby carrier market using beautiful and highly functional Scandinavian styling and including some very comprehensive features. Best Soft Structured Baby Carrier.
LILLEbaby The Complete Airflow is our favorite soft structured baby carrier. These are the best baby carriers of 2021. A soft-structured baby carrier also known as buckle hip carriers are probably the most popular and common type of carrier parents go for.
From faithful favourites to those that have just arrived in Canada we give you the best five SSCs. Baby can ride in. The Best Soft Structured Baby Carriers.
It has 3 carrier. Courtesy of Solly Baby. Tula Ergonomic Infant Carrier.
Soft-structured carriers come in a variety of styles and looks but essentially they all follow the same design. This lightweight carrier is perfect for parents on the go as well as those with babies who tend to be on the heavy side. Anyone who carries a baby frequently will tell you that a soft-structured carrier or SSC offers the best overall support and will help you carry your child for hours at a time.
Soft-structured carriers come in a variety of brands and styles and you can also get different accessories such as chew pads and headcovers to go with them. From bringing baby along for a hike to extra cuddle time find out which carrier is right for you. A soft-structured baby carrier is probably the most common type of carrier and is what comes to mind when many people think of babywearingIt has buckles that attach around the parents waist and back to secure the baby in the carrier.
Infantino Sash Wrap and Tie Baby Carrier Yet another recommended product in our list of the best baby carriers is the Infantino Sash Mei Tai. See our review of the best baby and toddler hiking carriers including reviews of Osprey Deuter Kelty Thule philteds Luvdbaby and ClevrPlus. The best baby carries like the Ergo 360 and the LILLEbaby carriers hold babys hips in that M formation to make front carrying safe.
The soft structured carries vary for ease of use between 4 and 7 depending on the number of straps and adjustment points and how hard they were to use when wearing the carrier with a baby inside. If youre expecting a baby and trying to choose among the many carrier options a buckle carrier also called a soft structured carrier or SSC offers a short learning curve and a backpack-like. This soft-structured carrier adjusts to fit a variety of body shapes and sizes.
Ergobaby 360 Baby Carrier. Available at Amazon starting at 33. Jessica Nellson February 4 2017 Soft-Structured Carriers Ergobaby Original baby carrier is one of the first models of carriers by ERGObaby.
The best soft structured carrier for newborn babies must be adjustable and versatile so you can use it for a long time without buying a new one every few months. Ergobaby is probably the best known soft structured carrier and for good reason. This best baby carrier has a wide waistband so it feels secure on your body a large fabric panel that keeps baby comfortably facing you or riding on your back and a ton of stylish.
This can make removing milk from your breast faster. Sweet almonds may promote breast milk production due to its potential estrogenic activity.
 10 Tips To Increase Breast Milk Supply Mommy On Purpose
10 Tips To Increase Breast Milk Supply Mommy On Purpose
Almonds offer vital nutrients such as protein calcium and healthy fats.

What helps to produce breast milk. Eat a Healthy Anti-Inflammatory Diet This healthy diet plan is heavy on fruits and vegetables whole grains like. Pump both breasts at the same time. Whey protein has lots of calcium as well.
Spinach and Beet Root Leaves. It has been said that you can do pumping sessions particularly between nursing sessions or you can do this after breastfeeding. Breastfeeding or pumping can make you quite hungry throughout the day so small meals can satisfy your hunger increase your energy level and help.
This is one of my favorites. Pumping both breasts will give you twice as much breast milk twice as fast in addition to helping stimulate more production. Look for foods naturally rich in zinc.
Breast milk provides your young baby with all the nutrients they need during the first months of their lives. Each breast should be pumped about 10 minutes. If you cant pump immediately after nursing try to pump halfway in between feedings.
You can try alfalfa tea which is made from dried alfalfa leaves. Nutritionists say it can help stimulate the production of breast milk and improve digestion and sleep. Caution must be taken when including dill in ones diet as it is a diuretic.
Dill is rich in iron magnesium and calcium. Flaxseed also contains essential fatty acids. Many doctors suggest new mothers to include fenugreek.
Creating a private and relaxing environment for breastfeeding and making the. Alfalfa is believed to be a galactagogue that helps lactating moms boost milk production. To produce breast milk you must consume enough calories to do so.
You can have sprouted alfalfa in soups. Both the plant and its seed fenugreek contain phytoestrogens Simpson writes which have long been believed to help milk production along. You can easily add fresh raw ginger to the dishes that you cook.
Consistent pumping between nursing periods will stimulate the breast milk production. You might experience vitamin deficiencies because of the amounts required to produce mothers milk. Fenugreek or methi seeds.
You can use it as a side dish to your main meal. The whole grain is a source of iron half a cup of dry oats has close to 2 mg of iron or around 20 percent of what breastfeeding moms need per day and low levels of the mineral are known to inhibit milk supply. Before you throw in the towel try these tips to boost your breast milk supply.
There arent any studies that show eating oats actually helps milk production though. Dill seeds can be used as such or in a ground form in pickles salads curries and cheese spreads. Fresh ginger is not only a healthy addition to your diet but it can also increase breast milk production and help with the let-down reflex.
But if you are pumping to produce milk faster you need to eliminate a huge amount of milk from your breast. Mix it with some kale and fruit and you have a delicious smoothie thats a perfect way to help increase your milk production. Asparagus can boost breast milk supply by helping to produce more breast milk by producing hormones that increase lactation.
You can eat a handful of almonds during midday add them to food as almond flour or almond butter or drink almond milk. There are also other ways to include these ingredients in other types of food to help improve lactation. Fennel fenugreek seeds Fennel is the vegetable with the white sweet licorice-flavoured bulb and thin green fronds.
It may be easier to consume smaller meals throughout the day instead of simply relying on the usual breakfast lunch and dinner. In its dried form goats rue is believed to be a safe supplement. Goats rue is a member of the same plant family as fenugreek.
Lactation cookies are special treats that contain several ingredients believed to increase breast milk such as brewers yeast fenugreek and oatmeal. Like sesame seeds flaxseed has phytoestrogens that can influence breast milk production. A simple internet search will produce several different recipes which will enable you to find the one that suits your taste buds best.
Anxiety stress and even embarrassment can interfere with the let-down reflex and cause you to produce less milk. A good way to keep your breasts stimulated is by pumping them. Alfalfa is the main food source for dairy animals to increase milk production.
5 However the fresh goats rue plant is dangerous and should never be used. The production of breast milk tends to be higher so pumping during this period is highly recommended. Usage of alfalfa to boost milk production.
The properties of this breastfeeding herb may help a mother to build up breast tissue and make more breast milk. Pumping at least 8 times during a 24-hour period will help to quickly increase breast milk production. Zinc is vital for breast milk production.
It is a rich source of Vitamin A Vitamin C and Vitamin K. However its also important to know about the vitamins to help produce breast milk including Vitamins B C and D. Flaxseed and Flaxseed Oil.
Studies indicate that fenugreek seeds have galactogogues which help in breast milk production in mothers postpartum.
As a mother you want to stock up certain foods that help increase breast milk supply. This is a great food to have on hand because its so versatile.
 Foods Supplements That Help Produce More Breast Milk
Foods Supplements That Help Produce More Breast Milk
Look for foods naturally rich in zinc.
/relactation-increase-milk-supply-431824-v2-45d5d6ac79294adc9f950964a3890e50.png)
Foods that help breast milk production. Taken in tea or in capsule form this herb generally increases milk supply within a few days. You should have at least one portion of green leafy vegetables on a daily basis. Protein is essential for the production of breast milk and it passes from the woman to the baby to nourish and support growth.
The whole grain is a source of iron half a cup of dry oats has close to 2 mg of iron or around 20 percent of what breastfeeding moms need per day and low levels of the mineral are known to inhibit milk supply. Green Leafy Vegetables Leafy vegetables like spinach kale fenugreek leaves and mustard greens are a great source of minerals such as iron calcium and folate. Fresh ginger is not only a healthy addition to your diet but it can also increase breast milk production and help with the let-down reflex.
It has been theorized that fenugreek stimulates sweat production and because the breast is a modified sweat gland milk ducts and milk ejection are stimulated. Some of the common foods believed to reduce breast milk are sage parsley peppermint and chasteberry. There arent any studies that show eating oats actually helps milk production though.
In addition to supporting milk supply it can also help you heal from the birth. Almonds are high in calcium so are edamame spinach kale and collard greens. Pumping milk from both breasts simultaneously has also been found to increase milk production and result in a higher fat content in the milk.
There is no conclusive evidence to prove that these food items are antilactogenic. Flaxseed and Flaxseed Oil. Just eat a balanced diet that includes a variety of vegetables fruits grains protein and a little bit of fat.
They contain properties that support the production of breast milk. Consuming too many candies a day might lead to drastic reduction of breast milk production in women. Cashews almonds and macadamia nuts are the most popular choices for giving your milk a boosttheyre also high in good fats and antioxidants.
These veggies have plenty of vitamins and are considered to help enhance the production of breast milk. Apart from peppermint tea many women love candies and altoids which are made of peppermint oil. Barley whole grain brown rice oatmeal and other foods made.
It can also be a snack. Brewers yeast is high in iron selenium chromium protein and B vitamins. Foods and Breast Milk You dont need to eat certain foods to make more milk.
Heres what you should be eating to increase your breast milk supply. Whey protein has lots of calcium as well. Like sesame seeds flaxseed has phytoestrogens that can influence breast milk production.
Its been used as a nutritional supplement for generations and has always been recommended as a milk booster. Consuming chicken eggs tofu and seafood has been associated with increased milk volume. 9 ways to help your body heal naturally after childbirth.
You can easily add fresh raw ginger to the dishes that you cook. However it passes easily into breast milk so you need to use it in small amounts to avoid gas or fussiness in your infant. Other foods that have potential to increase breast milk production.
Dill Apricots Asparagus Garlic Red beets Sesame seeds Poppy seeds Caraway seeds Anise seeds Coriander seeds. Flaxseed also contains essential fatty acids. For this reason breastfeeding women require an additional 25 grams.
Some antilactogenic beverages include alcohol and caffeinated beverages. Used around the world in cooking and baking fenugreek is a good source of protein iron vitamin C and more. Whole grains are very nutritious and great for lactating mothers.
Oatmeal provides mothers with an amazing variety of nutrients that can create a richer supply of milk. Plus eating protein-rich foods can help keep you full between meals. Take a breather grab a handful of nuts and enjoy a snack that will help your breast milk supply.
Must Have 31 Foods to Augment Breast Milk Supply in Lactating Mothers It is important for a lactating mother to make some alterations in her diet so that the vital nutrients get to the infants body in the natural way. Breastmilk Making Food 1. But regular consumption might lead to less breast milk production.
Mix it with some kale and fruit and you have a delicious smoothie thats a perfect way to help increase your milk production. Best of all its a food that can help increase breast milk supply. Its a cereal also a source of iron which can be a factor in low milk supply.
Fenugreek Fenugreek seed is a common herb for increasing milk production.
But without ovulation conception isnt possible. Generally the best chance of pregnancy is when sex happens 1-2 days before ovulation.
/1959936-why-cant-i-get-pregnant-if-im-healthy-5afb17166bf06900361243e6.png) Why Am I Not Getting Pregnant 8 Possible Reasons
Why Am I Not Getting Pregnant 8 Possible Reasons
We Asked a Doctor to Explain A surrogate mother thought she gave birth to twinsbut it turns out the boys were half-brothers.
:max_bytes(150000):strip_icc()/1960235-how-long-does-ovulation-last-01-5ae09af91f4e130039d80d9e.png)
Can you ovulate while pregnant. Lamb says that if youre on hormonal birth control you might not ovulate and sometimes you may ovulate but not experience any bleeding. Thats because sperm can live up to five days if its trapped in fertile cervical mucus. Does she use an ovulation monitor.
Ovulation is the act of your body releasing an egg and sometimes two or more during the menstrual cycle. Can a Woman Ovulate During Pregnancy. If this was possible it would mean that you would have two babies with different due dates.
Can You Ovulate While Pregnant. While most women realize that ovulation must occur in order to become pregnant many fail to recognize that waiting for ovulation to occur before they begin having sex can lead to them missing their most fertile window. AND NO YOU CANNOT HAVE A PEIRiOD WHILE PREGNANT.
Yes You Can Get Pregnant While Already Pregnant. With this definition of a period you cannot ovulate while on your period. In a creepy quirk of the human body under very exceptional circumstances a woman can continue to ovulate while pregnant and can conceive another child - something known as superfetation.
Ovulation tests are great for predicting when ovulation is going to occur to help you time intercourse and pregnancy tests are great for telling you if youre pregnant. Thats why confirming successful ovulation can tell you if you even have a chance at getting pregnant that cycle. Puberty menstruation pregnancy perimenopause and menopause.
Ovulating early may lower your chances of getting pregnant because there isnt as much uterine lining when an egg is fertilized making it harder for the egg to attach to the uterine wall. This can happen on lower-dose hormonal birth control like IUDs which dont suppress ovulation but do prevent buildup of the uterine lining therefore preventing you from getting a period. For example the pathway to the egg must be clear.
Once ovulation happens the egg that is released is only considered viable for 24 hours. A straightforward answer to the possibility of ovulation while being pregnant is a simple no. Having sex during this time gives you the best chance of getting pregnant.
But the most fertile days are the three days leading up to and including ovulation. Also you need sperm. In order to have a double pregnancy youd have to either ovulate while pregnant or have two uteri.
By 12-24 hours after ovulation a woman is no longer able to get pregnant during that menstrual cycle because the egg is no longer in the fallopian tube. The chances of getting pregnant come down as the woman crosses 35 years. Remember you can get pregnant right after your period even if youre not yet ovulating.
Ovulation is essential to getting pregnantbut it takes more than just an egg to conceive. Both of those scenarios again are highly unlikely. This egg then makes it away through the fallopian tube and if sperm is present there it will end up being fertilised.
Can You Ovulate During Your Period. But if you are hoping to get pregnant sooner rather than later just remember in those first three to five months of breastfeeding youre probably not going to ovulate because prolactin. Early ovulation is ovulating while youre still on your period which is very uncommon but possible.
Ovulation when being pregnant isnt possible because an egg cant get embedded into the uterus if there is already another egg there. But did you know confirming ovulation during the two week wait can tell you if you even have a chance at pregnancy. Ovulation could occur on any one day during this window.
If Youre Ovulating You Wont Have Trouble Getting Pregnant. These are the various stages in a womans biological cycle. So it behooves.
That means a woman can have two foetuses developing inside her at the same time both at different stages of development. The simple answer is no. GUESSING does not work the only way to know for sure is to use a monitor.
You cannot ovulate while you are pregnant. You can see that it is impossible to ovulate when you are already pregnant. You say she ovulated 4-5 days ago how does she know.
YOU CAN have BLEEDING which is LIKE a period and heavy but it is NOT TECHNICALLY A peirod. Track Your Most Fertile Days. In scientific terms ovulation is the process where the ovaries release an egg during a menstruation cycle.
If the fallopian tubes are blocked pregnancy cant occur. Getting pregnant isnt only about the womans fertility. The egg travels down the fallopian tube where it waits to meet with the sperm.
If you have a regular 28-day cycle count back 14 days from when you expect. Menstruation or a period is the bleeding that occurs when the endometrium is shed 12 to 16 days after ovulation. No you do not ovulate while pregnant.
One leads to the other while pregnancy can happen at any time during a womans years of fertility.
In newborns younger than 1 week black is a healthy color for stool. This is considered normal as long as there is no blood or mucus in the stool.
 Green Poop In Kids Causes In Babies Toddlers And Children
Green Poop In Kids Causes In Babies Toddlers And Children
Other symptoms of this might include skin rash like eczema or a red sore rash on your babys bottom gassiness fussiness excess spitting and blood or mucus in babys stool.
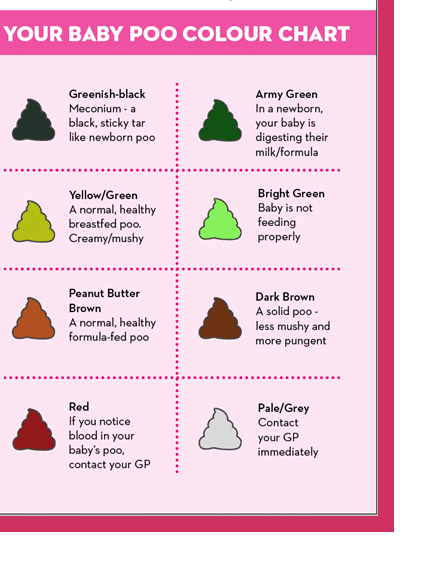
Green bowel movements baby. Various factors can cause changes in the color of a babys stools. Breastfed babies pass green poop if their moms eat a lot of leafy greens purple or blue-colored food and certain medicines. Diarrhea can also cause green poop.
The most common cause of green stool is baby food and is not cause for concern. Green poop is rarely a need for worry and in infants it. The baby may have a viral infection or may be suffering from stomach flu both of which lead to diarrhoea in the form of watery green stools.
If your baby is not getting enough milk he may be fussy and tensesometimes wanting to feed all day or he may be very sleepy and he will not be gaining much weight. Green poop indicates they arent getting the fat from breastmilk so only getting the watery milk at the beginning have a tongue tie check from your health visitor she says. Dark green stool is usually caused due to bile juices.
If your babys poo is green with slimy glistening streaks this normally means there is mucus in the poo. A change in poop color may happen when your baby is ill. Dark green poop baby poop color forest green.
Iron supplements are notorious for causing dark green stools. Green poop in kids is usually due to something that they ate such as leafy greens or food coloring. Foods that may cause dark green feces - green vegetables onion dill cabbage spinach lettuce broccoli licorice red beans chocolates with dyes fruit juices red meat muesli cereals sea fish.
If your baby has scant green poo not many dirty nappies and not much green poo in each nappy this can indicate insufficient milk intake. In breast-fed babies watery-green colored bowel movements are an indication that the infant isnt consuming enough high-calorie breast milk. These foods are super healthy but they can impart a green hue to your babys stools as well.
They might also be sensitive to a drug youre. When babies go through their teething phase they end up swallowing excessive drool and saliva which can lead to intestinal irritation. Your baby may have green poop if youre breastfeeding and taking medication when your baby is on medication or when she is ill with a stomach virus or cold for example.
Newborns who receive phototherapy for neonatal jaundice might have green poop as the excess bile is excreted through the stool 3. As a parent you need to carefully examine the color and texture of your babys bowel movement every now and then. Palmer a leading cause of green baby poop is a food intolerance either to something in the mothers diet or the babys formula.
Green poop in babies is completely fine as long as the baby is gaining weight. But in an otherwise healthy baby green poops are usually normal. This can hit his tummy too fast creating air bubbles and explosive green poos.
A mild illness can also change the color and consistency of an infants bowel movements and green colored feces in both breast-fed and bottle-fed babies can indicate a mild infection or a food intolerance. What you eat may be the reason of green poop in breastfed baby. Your babys poop could become green or have a mucus-like consistency because of a sensitivity to something in your diet though this is uncommon.
Mucus stomach bug and an imbalance in the foremilk and hindmilk can also cause green stool. Green poop in children. Bright green poop baby poop color lime green.
A formula-fed babys poop will normally be tan but because some formula is fortified with iron you may notice dark green poop. The number one ingredient that babies. Eating too much of greens and having too much of green drinks and foods including green sodas green gelatin and green sports drinks can change the color of your milk and in turn affect you babys poop color.
Diarrhea or other illnesses. Your baby may be gulping a lot of milk at once. Common colors and their causes include.
If youre breastfeeding green poop could also indicate a milk allergy or sensitivity to your diet. Do take the baby to the pediatrician if you find blood stains or streaks along with the green poop. Green poop in toddlers is not uncommon.
After consuming these products the stool may turn green within. Babies who become gassy cranky and cry after breastfeeding might be lactose intolerant. Your baby can relax and feed for as long as he wants comfortably supported by your body.
After the initial three days the sterile stool may turn yellow to green once the baby starts to digest the breast milk. Similarly supplements taken by you or by baby can turn stool green. If the baby has frequent green stools but at the same time is gaining weight the main reason is overload of lactose in the babys system.
Newborns pass a dark green or black stool called meconium an aggregate of everything they consumed in the womb. Spinach and other dark green leafy vegetables. This irritation leads to a green mucous-like stool.
You can try a laid-back feeding position to ease this problem.
While only a small percentage reaches your baby babies metabolize alcohol more slowly than adults. 5 fluid ounces of wine.
 How To Enjoy A Glass Of Wine While Breastfeeding
How To Enjoy A Glass Of Wine While Breastfeeding
Alcohol can be detected in your breast milk for about 6 to 8 hours after you have consumed the wine.

Breastfeeding glass of wine. Ingestion of alcoholic beverages should be minimized and limited to an occasional intake but no more than 05 g alcohol per kg body weight which for a 60 kg mother is approximately 2 oz liquor 8 oz wine or 2 beers. Nursing should take place 2 hours or longer after the alcohol intake to minimize its concentration in the ingested milk. It shouldnt affect your baby at all especially if you wait two to four hours after a single drink before you feed your baby.
Choose dry white wine with the lowest alcohol degree. A note on excessive drinking while breastfeeding While the occasional glass of wine or beer is perfectly fine for breastfeeding moms excessive alcohol can create problems for newborns. Since it takes your body 1 to 3 hours to metabolize.
Even a sip of wine can lead to severe consequences for the baby. If your baby is under 3 months old it will take them longer to process the alcohol as their liver is still developing. Dont drink alcohol during the first 3 months after giving birth.
Its not an either-or proposition. Rules for Drinking Wine during Breastfeeding. Large quantities of alcohol can cause weakness drowsiness deep sleep and abnormal weight gain in infants and excessive drinking can lead to failure to thrive.
While we know now that alcohol doesnt increase milk production and when abused can actually decrease supply there is no evidence that drinking in moderation harms your baby in any way. Both the Canadian Paediatric Society and the World Health Organization recommend exclusive breastfeeding for the first six months and up to two years. If youre sober enough to drive youre probably sober enough to breastfeed.
After consuming 3 glasses of wine or even more you can expect the following. If you choose to drink avoid breast-feeding until alcohol has completely cleared your breast milk. The American Academy of Pediatrics Section on Breastfeeding notes.
But never share a bed or sofa with your baby if you have drunk any alcohol. This typically takes two to three hours for 12 ounces 355 milliliters of 5 beer 5 ounces 148 milliliters of 11 wine or 15 ounces 44 milliliters of 40 liquor depending on your body weight. For example if a 175-pound woman consumes three drinks in an hour her body will take about six hours to clear the alcohol.
Breastfeeding moms are freaking entitled to a drink every now and then. Daily and heavy intake of an alcoholic drink may affect your breastfed baby negatively. A breastfeeding mom should limit alcohol intake based on her weight.
And seriously breastfeeding is lovely and amazing but it can be exhausting as all hell sometimes. Its also important to consider your body shape and size when you are enjoying a glass of wine. On average it takes about 2 to 3 hours for a glass of wine or beer to leave your system so its best to wait a few hours to breastfeed.
Generally moderate alcohol consumption by a breastfeeding mother up to 1 standard drink per day is not known to be harmful to the infant especially if the mother waits at least 2 hours after a single drink before nursing. Obviously the more you drink the longer it takes. The safest dose is no more than 2 oz.
But then they go on to say the American Academy of Pediatrics Section on Breastfeeding advises ingestion of alcoholic beverages should be minimized and limited to an occasional intake but no more than 05 g alcohol per kg body weight which for a 60 kg mother is approximately 2 oz liquor 8 oz wine or 2 beers. Nursing should take place 2 hours or longer after the alcohol intake to minimize its concentration in the ingested milk and that many experts recommend against drinking more. Having a glass of wine with dinner shouldnt be a problem at all it would put minuscule amounts of alcohol in your breast milk.
I hope this info has been helpful. Effects Of 3 Glasses Of Wine While Breastfeeding. Alcohol does pass into your breast milk in much the same way that it passes into your bloodstream and whats in your blood is in your milk.
Enjoy your baby enjoy nursing and for crying out loud enjoy a nice cold beer or a heavenly glass of wine when you feel like it. Alcohol that you drink while breastfeeding does indeed pass into your milk. They sum it up thusly.
But moderate alcohol consumption for breastfeeding moms is okay. Most experts dont want to see women abandon breastfeeding because they also want the occasional beer. For years doctors and midwives suggested having a glass of wine or beer to help you relax and produce more milk.
If the child is older than six months then you can have a glass. The alcohol percentage in your breastmilk is not the same as the alcohol in your bloodstream but it will peak about a half hour to an hour after you drink so a lot of sources recommend waiting two hours to nurse again. An occasional drink is unlikely to harm your breastfed baby.
I was told you rule was if you can drive you can breastfeed so 1 glass of wine is completely fine 2 might be pushing it but if you know when baby is going to next want a feed and its not for a few hours then youll be fine x. So just go with it. We have to cut mothers a bit of slack Pound says.
15 fl ounces of distilled spirits. Breastfeeding and drinking alcohol Anything you eat or drink while youre breastfeeding can find its way into your breast milk and that includes alcohol.
Can i use a suppository during. The relief you trust from PREPARATION H now with lidocaine and phenylephrine to numb painful hemorrhoid symptoms and reduce swelling.
Preparation H is considered safe while breastfeeding.
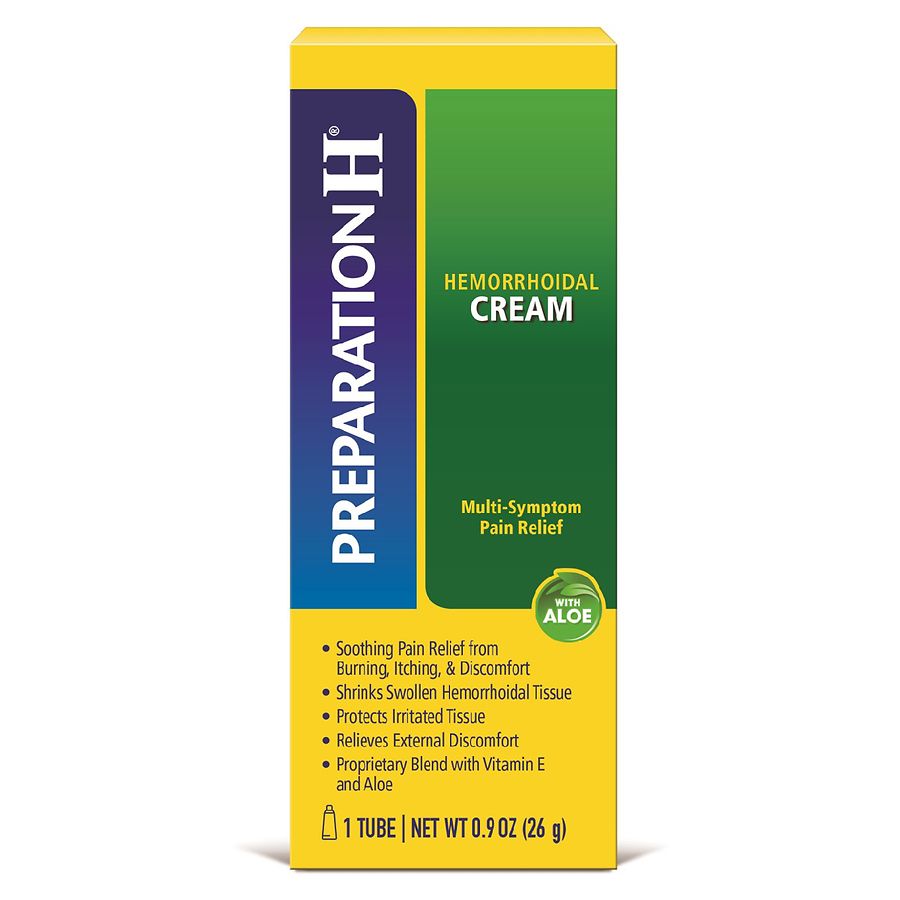
Preparation h and breastfeeding. Preparation H and breastfeeding. Mylanta Turns Maalox Rolaids Pepcid Prilosec Zantac. Preparation H Ointment use while Breastfeeding Important.
Breast milk storage bags or clean food-grade containers with tight fitting lids. Anyone know if its safe to use while breastfeeding. Controlled studies in pregnant women show no evidence of fetal risk.
Side effects of preparation h suppositories. Indigestion or heartburn Maalox Maximum Strength Chewable Tablets Mylanta Tums Pepcid AC. Can I take azo while breast feeding.
They can be. I am nursing and i think i have hemorrhoid i am worried if its ok to use preparation H. 2010 preparation-h-ointment-phenylephrine-mineral-oil-petrolatum-rectal-999740 Drugs Drugs.
At some point during your pregnancy or after childbirth you might have to deal with dry itchy skin around the anal area. Dont rub or scrub your nipples this will only hurt you and make breastfeeding difficult. Preparation H Soothing Relief Get that fresh butt feeling with NEW Preparation H Soothing Relief Cleansing Cooling Wipes daily wipes that go beyond cleaning to cool soothe and reduce irritation.
Hemorrhoids Anusol HC ointment Preparation H ointment or suppositories Tucks Pads. The hormonal changes pregnancy brings to your breasts are sufficient preparation for most women. Preparation H offers a range of products that contain natural ingredients and are suitable for use during pregnancy and breastfeeding.
Water pills while breast feeding. Is it okay to use Preparation H while breastfeeding. Pregnant or breastfeeding patients should seek advice of health professional before using OTC drugs.
My bottom was ready to move on from this dark episode of motherhood. I was relieved when I found out that there were no studies indicating that it passed from mother to infant via breast milk. Find everything you need to know about Preparation H Phenylephrine Rectal including what it is used for warnings reviews side effects and interactions.
Tuck it in your undies and sit. This information is not intended as a substitute for professional judgment. Preparation H Anusoll Anusol HC HeartburnIndigestion.
Please check each of the links below where breastfeeding lactation information is available. PREPARATION H Rapid Relief with Lidocaine Cream has a powerful combination of maximum strength lidocaine plus skin protectants that provide a soothing protective layer to offer relief of hemorrhoid symptoms. So yes Preparation H is safe while breastfeeding.
For maximum-strength itch relief try NEW Preparation H Soothing Relief Anti-Itch Cream with 1 Hydrocortisone in a soothing cream. IF you still have your epi foam from the hospital take a tucks and pump some epi foam on it. Learn more about Preparation H.
Bromfed Promethazine VC with Codeine Vicks DayQuil Severe Cold Flu Sudafed PE Congestion Neo-Synephrine Mucinex Fast-Max Severe Congestion Cough Dimetapp Childrens Cold Cough Cough Cold Relief Alka-Seltzer Plus Cold Norel AD Show all 1310. Boils while breast feeding. Teaching your baby the right way to latch on to your breast from the beginning is the most effective way to prevent soreness.
Available pack sizes Preparation H Clear Gel is available in 25 g and 50 g packs. Nausea Dramamine ginger vitamin B6 25 milligrams Sore throat chloraseptic throat spray or lozenges cough drops saline gargle. Use of preparation h while breastfeeding.
Preparation H Ointment is a drug containing multiple ingredients. Can you take theraflu while breast feeding. Preparation H is safe for pregnant women.
Preparation H Clear Gel is suitable for use during pregnancy and breastfeeding. Taking hoodia while breast feeding. Phenylephrine use while Breastfeeding.
It is commonly prescribed for external hemorrhoids. Medications that are Safe to Use during Pregnancy and Breastfeeding This is a list of over -the-counter medications that can be safely taken while pregnant and breast feeding. I was thrilled in the least.
Your hands well with soap and water. Its going to sting like a beeyatcha for a minute or two and then it will be sweet cooling relief. I have a huge hemorrhoid that is just getting more aggravated from all the.
Inspect the pump kit and.
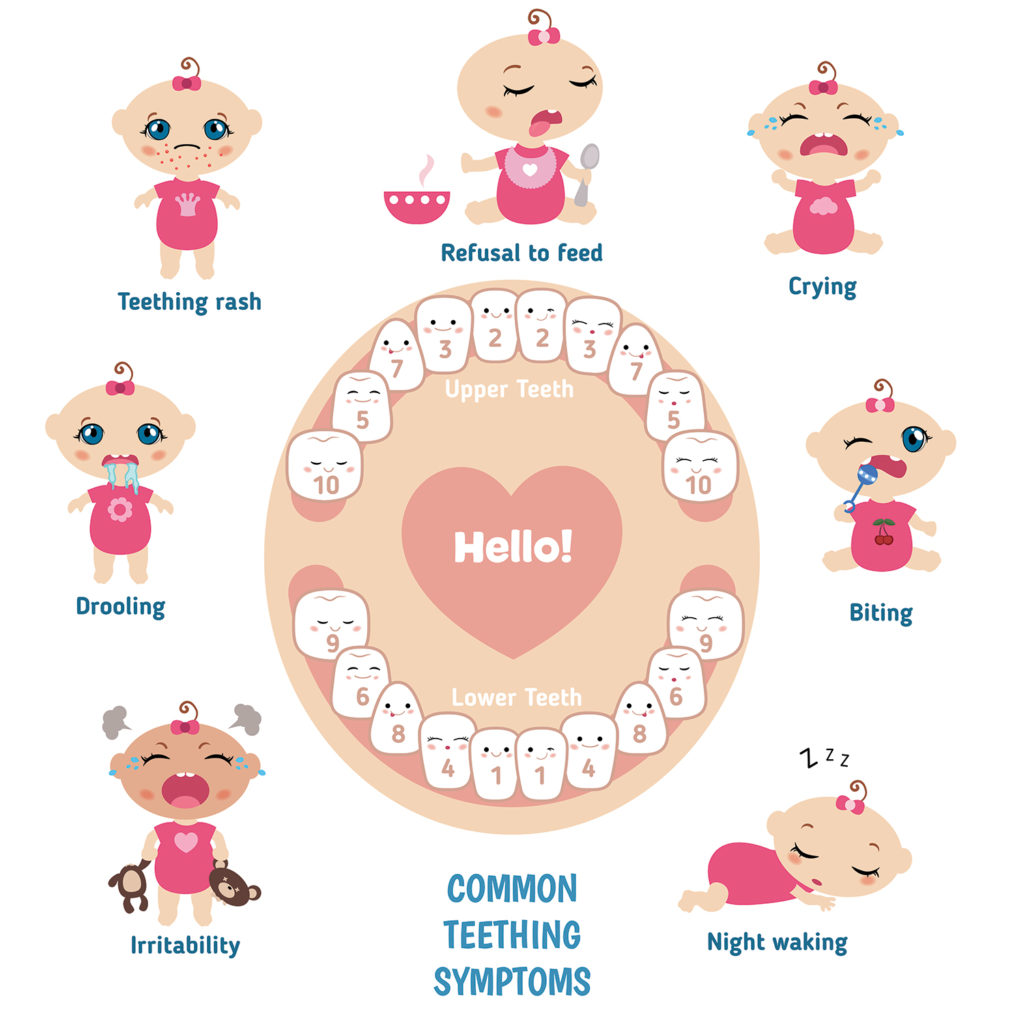
And these symptoms occur about four days before and up to three days after your babys tooth comes in although the more bothersome symptoms including decreased appetite not sleeping rash and ear rubbing are most common on the day the tooth actually erupted or a day or two beforehand. If you arent sure whether your baby is teething or not ask your childs healthcare provider for personalized advice.
 Four Signs Of A Teething Baby Anchorage Pediatric Dentistry
Four Signs Of A Teething Baby Anchorage Pediatric Dentistry
Teething is the process by which a babys teeth erupt or break through the gums.

Symptoms for teething babies. If your baby has these symptoms see your pediatrician. Red flushed cheek or face. They are rubbing their ear.
Check for symptoms of teething like fussiness excessive drooling or sore red gums. Understandably many parents wonder when their babies will start teething as it is known to be a tumultuous time for both the infants and parents. Increased fussiness or irritability.
Call your doctor if your baby has diarrhea vomiting rashes on the body a higher fever or cough and congestion. If your baby is 6 months or older you can give them healthy things to chew on such as raw fruit and vegetables. Baby teeth sometimes emerge with no pain or discomfort at all.
On the other hand a higher rectal temperature over 1004F 38C vomiting or diarrhea are not usually signs of teething. For each tooth that is emerging teething symptoms can last up to several days. Making matters more challenging symptoms can vary based on the child age tooth and daytime versus night.
They are gnawing and chewing on things a lot. Teething generally occurs between 6 to 24 months of age. Your baby is dribbling more than usual.
Symptoms and remedies for Baby teethingWhat should we do while baby teethingbachhe ki daant nikalte samay kya karna chaiyeaur sabhi doubts clear karein i. You could also try giving your baby a crust of bread or a breadstick. Increased Drooling Babies drool a lot but when they start teething or their teeth start to emerge their drooling increases.
Symptoms of teething often occur a few days or even weeks before the tooth comes through the gum. While many parents assume this means their child is teething it could still be months until that first tooth erupts. In most cases though it would be very rare if your baby does not experience at least a few of these signs when teething.
The common symptoms are. A tooth visible below the gum. One cheek is flushed.
Your babys gum is sore and red where the tooth is coming through. Red and swollen gums. Common signs of teething are.
Signs that your baby is teething. Slight increase in temperature but no fever. But most babies start teething at around 6 months.
Teething can be painful but it doesnt usually make babies sick. One of the signs that your baby is teething is that they start to chew on their fingers toys or other objects they get hold of. Sore or tender gums.
How to Soothe a Teething Baby Your child may have sore or tender gums when teeth begin to erupt. Irritability Babies become fussier and irritable when they are teething. The trick is.
Some of the most common symptoms of teething in babies are. Trying to bite chew and suck on everything. Many parents suspect that teething causes fever and diarrhea but researchers say these symptoms arent indications of teething.
Rubbing face or pulling hair. There are judgments like teething cause pain common cold fever and diarrhea but there is no scientific evidence to support any connection between these symptoms and teething. If your baby has any of these symptoms while teething and continues to be cranky and uncomfortable call your pediatrician.
Drooling which can cause a facial rash Swollen sensitive gums. Some of the most common signs and symptoms of teething include. The symptoms of early teething are exactly the same as right-time teething.
Other babies may not display any signs or symptoms related to teething. Symptoms of teething include irritability tender and swollen gums and the infant wanting to place objects or fingers into the mouth in an attempt to reduce discomfort. Classic signs and symptoms of teething include.
Pieces of apple or carrot are ideal. You might see some crankiness and a lot of tears but you can make this transition easier for your baby. 1 Increased Biting We all know how curious babies are and how they seem to want to chew on everything they can get a hold of.
Common symptoms and signs include. At other times you may notice. Gently rubbing their gums with a clean finger a small cool spoon or a moist gauze pad can be soothing.
How Common Are Lip Ties. Someone who has tongue-tie might have difficulty sticking out his or her tongue.
Laser Tongue Tie And Lip Tie Procedures Associates In Pediatric Dentistry
Wood block courtesy of Dr.

Lip and tongue tie. Where this doesnt happen the frenulum may restrict tongue mobility. Tongue-tie can also affect the way a child eats speaks and swallows. These include orthodontic issues dental decay speech problems and esthetic problems.
Though most infants have some degree of upper lip tie when it becomes large and tight enough it may prevent the upper lip from flaring out or curling up which is essential for breast-feeding in order to create an adequate seal with the breast. If a lip-tie was released you may notice some swelling of the lip for a few days after the procedure. That said a lip-tied baby can have trouble breastfeeding because its.
Lip tie is a similar condition involving the band of tissue that connects the upper lip to the gum. Tongue-tie ankyloglossia is a condition present at birth that restricts the tongues range of motion. Aside from future speech difficulties and distress to whenever eating certain types of food in the short term lip and tongue tie causes trouble with the feeding and development issues.
Tongue ties may have an impact on breastfeeding eating and speech. Ghaheri an ENT at the Oregon Clinic says a lip tie is much less common than a tongue tie a condition where a short tight piece of tissue below the tongue restricts its range of motion. Tongue-tie ankyloglossia occurs when the band of tissue frenulum that connects the tongue to the floor of the mouth is short tight or thick resulting in restricted movement of the tongue.
There are potential problems for infants with unrevised lip and tongue ties. Some of the complications associated with a lip tie are. A tongue tie is also more likely to affect breastfeeding because the tongue is unable to move up.
There are two frena found in the midline under the upper and lower lips. Once you lift the lip look for a band of tissue that connects the lip to the gum area. This may make it more difficult to move the upper lip.
Tongue tie with lip tie can make breastfeeding difficult for babies and in some. As an adult a lip and or tongue-tie can cause periodontal disease esthetic problems with smile lines and poor oral hygiene. Related to tongue tie and its posterior hidden variant which may cause problems with breast-feeding upper lip tie is when the upper lip is tethered to the upper gum.
Tongue and lip ties often occur in tandem are more common in boys than girls and tend to run in families. Many physicians do not properly assess for tongue or lip-tie or recognize their impact on the breastfeeding relationship leaving babies vulnerable to early weaning. Lip tie has not been studied as much as tongue tie but treatments for lip ties and tongue ties are very similar.
Tongue tie ankyloglossia is caused by a tight or short lingual frenulum the membrane that anchors the tongue to the floor of the mouth. Jakarta - Selain tongue tie bayi baru lahir juga berisiko mengalami lip tie. Tongue and lip-tie are common causes of nipple pain uneven breast drainage slow weight gain and low milk supply.
The frenulum normally thins and recedes before birth. Dikutip dari Standford Children Health biasanya jika tongue tie ditemukan pada bayi yang lebih kecil prosedur menggunting frenulum atau disebut dengan frenotomy bisa dilakukan jika anak yang sudah lebih besar bisa melalukan frenuloplasty. A lip tie occurs when the labial frenulum which is the piece of tissue that attaches the upper lip to the gums is very tight.
The discomfort from lip and tongue-tie release usually only lasts for about 24 hrs although in older children the discomfort may last about 48 hrs. 7 Tips Sukses Menyusu Bayi dengan Tongue Tie dan Lip Tie. Oral issues like tongue and lip ties develop in the womb as a result of a gene mutation passed on as a dominant trait.
Wood block of a physician performing a frenectomy dated 1679. This is known as a lingual frenum. Kondisi ini kadang-kadang juga memerlukan tindakan serupa tongue tie seperti frenotomi.
Now lets look for the source of many nursing problems including the lip callus a maxillary tie aka lip tie. There is also buccal ties which involve the cheeks. At KIDS our mission is to help everyone to get the best possible bond together.
With tongue-tie an unusually short thick or tight band of tissue lingual frenulum tethers the bottom of the tongues tip to the floor of the mouth so it may interfere with breast-feeding. Ankyloglossia also known as tongue-tie is a congenital oral anomaly that may decrease the mobility of the tongue tip and is caused by an unusually short thick lingual frenulum a membrane connecting the underside of the tongue to the floor of the mouth. If the frenulum aka the band of tissue is tight a lip tie is likely.
The most problematic frenum is found in the midline under the tongue. A lip tie is an unusually tight labial frenulum which keeps the upper lip tethered to the gum line. When this frenum prevents correct tongue function it is commonly known as tongue-tie or ankyloglossia.
Lip and tongue tie affects around 5 of Australian newborns. A baby born with a tongue-tie or ankyloglossia will have an overly short or.
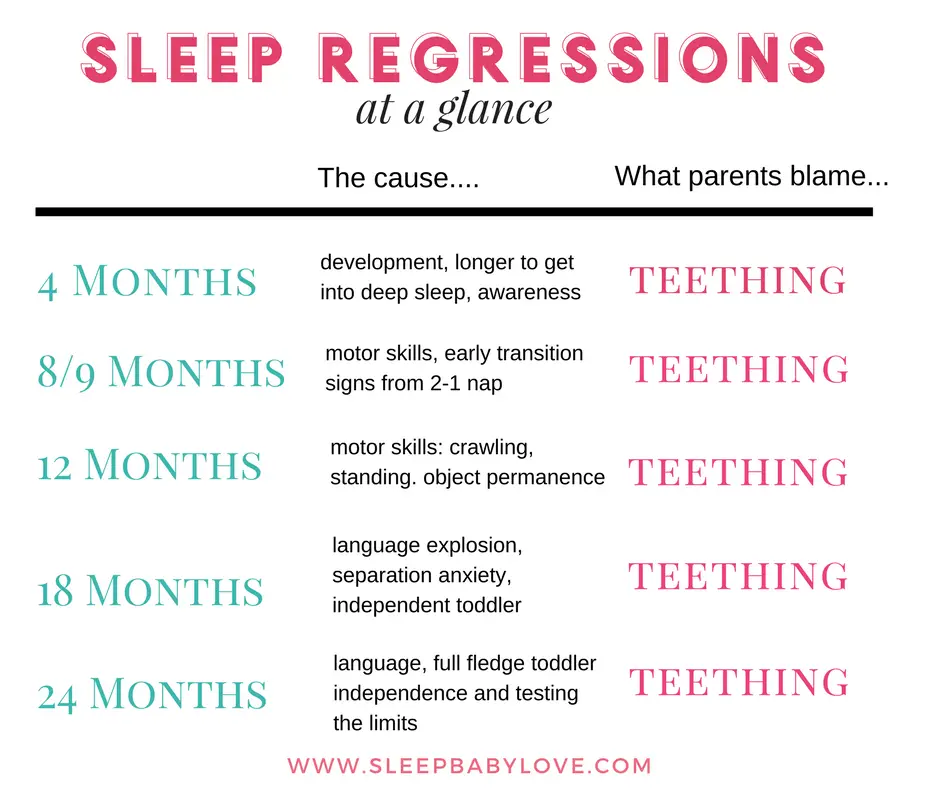
While those sleep regressions typically last a few weeks the 4-month regression may mark a permanent change in the babys sleep pattern. Your little one is understandably eager to practice her new skill which can leave her restless and prone to waking up more often than normal.
 Try To Survive A Sleep Regression With These 5 Tips Sleep Baby Love
Try To Survive A Sleep Regression With These 5 Tips Sleep Baby Love
Babies may begin sleeping less deeply at 4 months making.
4 month old baby sleep regression. These regressions seem to come out of nowhere and can last indefinitely. While it may feel like an eternity 4-month sleep regression can last anywhere from two to six weeks. So in general its when someone is experiencing a disruption in their sleep for longer than a few days.
For some babies the 4 month sleep regression is relatively mild and very brief. The 4-month sleep regression could begin as early as 3-months-old or as late as 5-months-old. The parent or the baby.
When does the 4 month sleep regression end. The 4 month sleep regression peaks for around 2-3 weeks. The most common age is 3 months to 4 months old.
Welcome to the very common Four Month Sleep Regression. But its also completely normal and most importantly its temporary. They result from a permanent change in sleep architecture.
The two- to six-week time period is the time it typically takes a baby to learn how to self-soothe and not wake up in the middle of the night as much. As we know all babies are different. The 4 month sleep regression can start any time after 8 weeks old though some babies dont sleep well from birth.
There are several culprits behind baby sleep problems at this age. Not all children go through sleep regression some babies start sleeping easily at night and never look back. Any type of sleep regression in children or even adults is just awful.
Causes of the 4-month-old sleep regression Sleep regressions including the 4-month sleep regression are usually the result of your baby passing through a big developmental milestone. Sleep regression is the time when your babys sleep patterns shift they wake up. If you keep this up for a day or two and notice your baby doesnt want to feed at these times then its likely a sleep issue not a hunger one.
Your baby will go through a number of sleep regressions in the first 2 years of their life the biggest being the 4-month sleep regression. At Baby Sleep Science we dont like the term four-month regression because the changes in sleep that occur around 34 months old arent really a regression at all. A babys first period of sleep regression typically occurs between when theyre three and five months old and is most commonly referred to as the four-month sleep regression In addition to disrupted sleep patterns other signs of the four-month sleep regression may include fussiness waking up multiple times during the night.
Changes in sleep are caused by a biological change in the way a child sleeps at this age rather than a regression. This regression can also start as late as 5 months. But when its with a four-month-old baby its hard to tell who has it worse.
One of the major ways the 4 month old sleep regression shows itself is by babies waking up after only 45 minutes. Its those brief awake periods that can cause a lot of disruptions to sleep and lead to the dreaded 4-month regression We put quotes around the word because we view it as somewhat of a misnomer. 3 to 4 months.
This is due to the change in sleep cycle length and often over tiredness from the short day time naps. What is sleep regression anyway. Sleep regression can happen any time during the baby and toddler years except during the newborn period.
Sleep regression at 4 months is a real thing. This is a natural and normal change for your baby but it can be a distressing time for parents. The dreaded 4-month sleep regression is often the hardest for parents simply because its the first.
Multiple night wakings especially if your baby has just begun to sleep longer stretches during the night Reduced naps or disaster naps Changes in appetite. Some indicators that youre experiencing the 4 month sleep regression are. Recognizing the 4 Month Sleep Regression.
The pain caused by teething hunger linked to growth spurts and the excitement of rolling over for the first time. A Typical Four Month Old Babys Sleep On Becoming Babywise describes four month olds as beginning to extend their morning wake times and complete five feed-wake-sleep cycles throughout a typical day. Once this 4-month sleep regression hits and your babys night sleep patterns change babies often start to wake every 2-4 hours overnight.
Assume that baby is hungry and simply feed baby as soon as he wakes. There is thought to be a regression around 34 months 9 months and 18 months. When a baby is born sleep is immature and nearly constant.
However parents commonly report problems with their childs sleep patterns at 4 months 9 months and 1 year old. A sleep regression is thought to occur when a baby who is normally sleeping well begins to wake frequently at night andor fightsrefuses naps. A recent study by researchers at Wayne State University published in The Journal.
For others the 4 month sleep regression is a very very rough phase marked by lots of crying and that lasts pretty much indefinitely. Its more about when your babys sleep cycle starts changingfor most its right around the 4-month mark but it could be a little earlier or a little later. For most babies the 4 month sleep regression occurs right around the 4 month mark but for some babies it happens a bit earlier around 3 months or a bit later around 5 months.
This is a common experience and so women should never feel ashamed for missing their pills or for having a pregnancy while using birth control Heres what you need to know about the risks of getting pregnant while using birth control. However because most women occasionally forget or miss their dose the realistic odds of pregnancy are higher about 9 in 100 9.
Theyre about 99 effective when you take them correctly.

Chances of pregnancy on the pill. While the pill is 987 effective against pregnancy there are those rare cases of perfect and consistent use and the pill still failing and a woman conceives. That means that one in every 100 women taking the Pill could become pregnant. The Birth Control Pill Oral contraceptives contain hormones that stop ovulation.
Even so between 2 and 8 percent of women become pregnant each year while using it. The risk of having unprotected sex and getting pregnant three days prior to ovulation is 15. If either of these happen the small amount of sperm in the pre-ejaculate might cause pregnancy even though the chances are small.
But thats if you take them perfectly meaning at the same time each and. When taken within 72 hours it may reduce the chances of getting pregnant by 89. Depending upon how many pills you have missed and when your chances of getting pregnant may.
It does this by stopping ovulation which means an egg isnt released from your. The IUD which is a small piece of flexible plastic thats inserted into your uterus by a doctor is 99 percent effective and prevents pregnancy from three years up to 12 years depending on the type and brand of IUD. If you start taking the pill right after your period ends youre good to go.
Getting pregnant while on birth control pills. The typical use rate meaning taking into account the imperfections in taking the pill as prescribed can reduce the effectiveness of birth control pills to about 91. This is a 30 chance.
Again this pill does not stop you from getting pregnant after you take it. Becoming pregnant while on birth control does increase your risk of ectopic pregnancy. This means that less than 1 out of 100 women who take the pill would become.
Consistent use lowers the chances of getting pregnant on birth control pill down to 1 which means 1 in every 100 women is getting pregnant on while on the pill every year. Being even 12 hours late in taking your birth control pill can increase your chance of getting pregnant. Although birth control pills have a high success rate they can fail and you can get pregnant while on the pill.
Planned Parenthood estimates that when taken perfectly the pill is 99 percent effective at preventing pregnancy. According to the Centers for Disease Control and Prevention CDC the pill is 997 percent effective with perfect use. If taken within 24 hours you can reduce the risk of pregnancy by 95.
You will have the highest risk of pregnancy by having unprotected sex one or two days before your ovulation starts. When the ovary releases the egg. Certain factors increase your risk of getting pregnant even if youre on.
The birth control pill is popular with Canadian women. If you start your pill on a random day in the middle of the month you need to use a backup for the first seven days. Birth control pills are considered effective but not foolproof.
If you have unprotected sex after taking the pill you may still get pregnant. But if youre using the pill correctly its highly unlikely that you can get pregnant this way. An ectopic pregnancy occurs when a.
The pill is up to 997 effective at preventing pregnancy when its taken correctly. The chances of getting pregnant on the pill while relatively low can increase if a woman does not use them consistently. If you use them perfectly theyre a great way to prevent pregnancy with a 997 effectiveness rate.
The pill is 99 percent effective in preventing pregnancy. You will have a 12 chance on the ovulation day. If you test positive you should stop taking your birth control pill.
MYTHS BUSTED Contraception options explained from the Pill implant and injection to the coil and condoms here are. In other words it can increase the risk of a possible pregnancy by up to 9 on average.
Choices for common infections. Rarely mastitis is seen in lactating pseudopregnant bitches.
 Infectious Lactational Mastitis Insights Into Breast Milk Microbiome Fx Medicine
Infectious Lactational Mastitis Insights Into Breast Milk Microbiome Fx Medicine
Fact sheet for Health Care Professionals Health Service Executive Ireland 2017 a review article Acute mastitis Blackmon 2020 and the BMJ Best Practice guideline Mastitis and breast abscess BMJ Best Practice 2020.

Best antibiotic for mastitis. Other oral antibiotics that may be used are amoxicillin and clavulanate combination ciprofloxacin clindamycin trimethoprim and sulfamethoxazole. Micotil is still the drug of choice considering both anecdotal and published reports. Your doctor may recommend an over-the-counter pain reliever such as acetaminophen Tylenol others or ibuprofen Advil Motrin IB others.
The prevalence of mastitis in breastfeeding women may reach 33. The goal of treatment for mastitis is to provide prompt and appropriate management to prevent complications such as a breast abscess. Inpatient therapy for severe infection without risk of MRSA.
Mastitis inflammation of the breast tissue is a common problem for breastfeeding women. The following information is a consensus guide. And both are active against beta-lactamase-producing Staphylococcus aureus and are indicated for soft tissue infections caused by S.
It is intended to aid selection of an appropriate antibiotic for typical patients with infections commonly seen in general practice. Based on this review and all available data the best option was found to be extended intramammary therapy for 5-8 days with Pirlimycin Pirsue. Identifying and managing predisposing factors for mastitis including poor infant attachment nipple damage smoking andor an underlying breast abnormality.
Patients with a breast abscess are referred to a surgeon for definitive care. A range of antibiotics are used to treat mastitis that occurs as a result of bacterial infection. Inpatient therapy for severe infection with risk of MRSA or in patients with beta-lactam.
The majority of women with mastitis can be managed in the home either with oral antibiotics or with intravenous IV antibiotics under the Home Hospital program. Mastitis is inflammation of the mammary glands associated with bacterial infection. When antibiotics are needed those effective against Staphylococcus aureuseg dicloxacillin cephalexin are preferred.
Both Flucloxacillin and Dicloxacillin are narrow-spectrum penicillins. Breast infections cause the breast to get red and inflamed swollen and tender to the touch. Mastitis can be caused by ineffective positioning of the baby at the breast or restricted feeding.
Nafcillin or oxacillin or ampicillin-sulbactam. It occurs in postpartum bitches and less commonly in postpartum queens. When antibiotics are needed those effective against Staphylococcus aureus eg dicloxacillin cephalexin are preferred.
Antibiotic therapy should be given for 10 to 14 days to help prevent recurrence. In refractory cases an ultrasound should be performed looking for possible underlying abscess a biopsy should be considered and cultures should be performed to exclude atypical micro-organisms andor. The best antibiotics to treat the infection caused by this bacterium are dicloxacillin cephalexin etc.
What Is The Best Antibiotic For Mastitis. Neonatalpaediatric mastitis treatment is best managed by a paediatrician. Flucloxacillin and dicloxacillin are the antibiotics of choice for mastitis according treatment guidelines 1 2.
When antibiotics are needed those effective against Staphylococcus aureus eg dicloxacillin cephalexin are preferred. Cephalexin and dicloxacillin are two of the most common antibiotics chosen but a number of. Mastitis can be caused by bacteria viruses and fungal microbes and can affect one or both of the breasts.
If your mastitis doesnt clear up after taking antibiotics follow up with your doctor. The recommendation to use paracetamol or NSAIDs for analgesia in women with mastitis is based on expert opinion in the Health Service Executive Ireland Mastitis. Prescribing oral antibiotics if indicated.
Although it can be associated with bacterial infection this is rarely its primary cause see milk stasis not infection is the main cause of mastitisMany doctors nevertheless choose to treat it with antibiotics just in case infection is present. Aureusbecomes more common it is likely to be. Aureus becomes more common antibiotics that are effective against this organism may become preferred.
It is specifically licensed for ewe mastitis and highly effective because it has good activity particularly within udder tissue and against the bacteria that have accumulated within inflammatory cells. Risk factors for developing mastitis include poor sanitary conditions trauma inflicted by offspring and systemic infection. Infective mastitis is commonly caused by Staphylococcus aureus.
Effective milk removal pain medication and antibiotic therapy have been the mainstays of treatment. Offering appropriate advice on measures to prevent recurrence such as encouraging good breastfeeding technique and maintaining good hygiene. Baby to keep breastfeeding or mother to continue to drain the breasts with a.
Aureus becomes more common it is likely to. There was no evidence to support the use of injectable antibiotics at the same time as intramammary therapy mastitis tubes used in the quarter to increase cure rates. For simple mastitis without an abscess oral antibiotics are prescribed.
The bacterium responsible for causing infection in mastitis is generally staphylococcus aureus. The acute breast abscess. Alternatively other antibiotics with activity against MRSA may be used but experience with these other agents in treating mastitis is limited.
Fenugreek is a rich source of protein iron vitamin C which helps maintain breast milk production. Native to the Mediterranean and Asia this herb is known for its maple syrup smell and bitter burnt sugar taste.
 Natural Remedy To Increase Breast Milk Production For Android Apk Download
Natural Remedy To Increase Breast Milk Production For Android Apk Download
Put the leaves in a.

Natural remedies for milk production. Fennel seeds are great for increasing the milk supply in nursing mothers. They are also rich in copper. A natural remedy may be one of the first things to try to increase your milk supply especially if you are hesitant about taking supplements.
They are good sources of phytoestrogen and also exhibit galactagogue properties in nursing mothers 1. Fenugreek contains phytoestrogens which appear to bind with estrogen receptors and thereby increase not only breast milk production but also sweat gland activity. Among the best home remedies for boosting milk production are fenugreek cumin seeds warm compress and more.
Some natural ways to boost supply shared below. These tips are informational only and not to replace medical advice with your physician. Fenugreek is the herb used most often to increase breast milk supply 1 and is the primary ingredient in many lactation teas.
A 2011 study tested 66 mothers. In general follow the manufacturers instructions. They also contain a decent amount of plant-based proteins which help make milk.
Cabbage leaves are very effective in drying up breast milk. Fenugreek seeds are an effective home remedy to increase breast milk supply. However you can reduce milk production and can dry up milk supply by following some home remedies which are given below.
It is believed that it stimulates sweat gland activity. It stimulates sweat gland activity mammary glands are modified sweat glands. Excess production of breast milk is blocked by the action of green gram paste which acts as a poultice.
Applying green gram paste on the breasts helps reduce the production of milk and helps the hyper lactating mothers by reducing the flow enough to feed the baby only. When youre breastfeeding you need to consume plenty of calories to give your body energy to make milk and whole grains are a healthy way to do so. Fenugreek contains phytoestrogens that help increase breast milk production.
Galactagogue is just a fancy word for foods or drugs that increase the production of breast milk. It has phytoestrogens similar to estrogen which is a hormone that also helps in producing more milk. Luckily for us mamas there are quite a few ways to help maintain and boost milk production so our little ones stay milk drunk.
Mammary glands are modified sweat glands. An age-old remedy is applying chilled green cabbage leaves over the breasts and replacing them every 2 4 hours as they wilt. Some manufacturers sell capsules or tinctures that contain fenugreek and blessed thistle together as well as other herbs for milk supply in some brands.
Across different cultures the ancient wisdom of using herbal remedies for postpartum support and breastfeeding has been handed down from generation to generation. Healthy whole grains like brown rice and quinoa can help with breast milk production for a number of reasons. Find out how to increase breastmilk supply fast and what foods to eat to produce more breastmilk.
Due to their high calcium content the intake of black sesame seeds is believed to increase breast milk production. Multiple studies have also found that fenugreek Trigonella foenumgraecum increases breast milk production. This will prove to be highly beneficial.
Poor breast milk production is the most common cause of breastfeeding failure. Green gram is one of the best home remedies to decrease breast milk. These ayurvedicnatural remedies are safe for mothers to try to improve the production of breast milk.
Fenugreek and Torbangun boosts milk production. Because the herbs are combined in one capsule or liquid tincture these types of products are a good. Home Remedies and Natural Tips to Stop Breast Milk Secretion You can express just enough milk to decrease the fullness and pain and then apply cold packs to the breasts.
Cabbage leaves may suppress lactation when used for long periods of time though more studies are needed. Fenugreek seeds are one of the best ingredients that can increase breast milk supply. Smoking and drinking moderate to heavy amounts of alcohol can lower your milk production.
Fenugreek is considered a good remedy for stimulating the milk-producing glands. Place clean and chilled cabbage leaves in your bra making sure the leaves are flat against the surface of the breast. Take apart and wash the leaves of a green cabbage.
Please note that this is not medical advice and if you have a concern about your milk supply it is best to discuss your concern with your doctor pediatrician and lactation consultant. One way of cooking it is in combination with lentils.
As a breastfeeding mother you should also check out the LactMed app and website before taking any type of treatment. If youre taking a medication that could be harmful to your baby your health care provider might recommend an alternative medication.
 Is It Safe To Take Claritin Loratadine While Breastfeeding
Is It Safe To Take Claritin Loratadine While Breastfeeding
On the bottom line loratadine is safe to use while breastfeeding.

Can you take loratadine while breastfeeding. If you are looking for a safe antihistamine to take while breastfeeding Claritin loratadine is recommended. Can you take loratadine with any other allergy medicine. Still a few medications arent safe to take while breast-feeding.
Its generally safe to take loratadine during pregnancy and while breastfeeding. These is no problem with Claritin loratadine and breastfeeding. Your doctor or pharmacist can give you.
The ingredients of Claritin Claritin-D Clarinex Allegra Allegra-D and Zyrtec are generally regarded to be compatible with breastfeeding again always double-check the active ingredients. Can You Take Antihistamines While Breastfeeding. Claritin-D 12 Hour is a drug containing multiple ingredients.
Most breastfeeding mothers are always concerned about taking any kind of medication as they are worried that it will be transferred to their babies through their breast milkWhile there are warnings on most antihistamine medications to caution nursing mothers some are safe to use while you are breastfeeding. Claritin shows extremely low concentrations in the breastmilk and lacks the sedative effects of first generation antihistamines. On this platform you will find all the information you need about all the medicine available in pharmacies.
The British Society for Allergy and Clinical Immunology recommends loratadine at its lowest dose as a preferred choice if an antihistamine is required during breastfeeding1 Drug Levels After a single oral dose of 40 mg of loratadine in 6 women average peak milk levels of 292 range 204 to 39 mcgL occurred at two hours after the dose. One Caution Watch carefully however if using Claritin-D. James DuRant answered 10 years experience Pediatrics Yes.
Because of its lack of sedation and low milk levels maternal use of loratadine would not be expected to cause any adverse effects in breastfed infants. Feel free to treat your allergies while breastfeeding. If you are worried about any symptoms that baby has contact the childs healthcare provider.
This information is not intended as a substitute for professional judgment. Loratadine might have a negative effect on lactation especially in combination with a sympathomimetic agent such as pseudoephedrine. The American Academy of Pediatrics recommends Loratadine while breastfeeding.
But try harmless remedies such as steam inhalation or anti-inflammatory herbs. Claritin-D 12 Hour use while Breastfeeding. Loratadine Claritin has been studied and the amount of loratadine that passes into breastmilk is extremely low.
View 1 more answer. As per the recommendations of the British Society for Allergy and Clinical Immunology loratadine can be taken at its lowest dose while breastfeeding. If you need an antihistamine while pregnant loratadine can be used but only if the benefits outweigh any risks and only if its prescribed by your doctor.
This along with the low levels in milk makes loratadine one of the preferred antihistamines for use during breastfeeding. Loratadine does pass to the infant in breast milk. Yes it is safe but within limits.
It passes into breast milk in low amount but has a minimal sedative effect. For more information about how loratadine can affect you and your baby during pregnancy read this leaflet on the Best Use of Medicines in Pregnancy BUMPS website. These is no problem with Claritin loratadine and breastfeeding.
There is iTune app or Android app for checking out any known side-effects of any medications while breastfeeding. Loratadine Claritin has been studied and the amount of loratadine that passes into breastmilk is extremely low. Always consult your physician.
When Loratadine Claritin they found that the amount of loratadine that passes into breast milk is extremely low and had almost no effect on babies. Can I take Loratadine while breastfeeding. Please check each of the links below where breastfeeding lactation information is available.
If your doctor prescribes loratadine while breastfeeding keep a watch on the side effects. Also the benefit of continuing to take a medication for a chronic condition while breast-feeding often outweighs any potential risks. If you are concerned about taking an antihistamine while breastfeeding talk to your obstetrician about alternative medications or means of treating allergy symptoms.
Feel free to treat your allergies while breastfeeding. Send thanks to the doctor. Compared to some other antihistamines loratadine has less chance of causing drowsiness for the mother or the baby.
The ingredients of Claritin Claritin-D Clarinex Allegra Allegra-D and Zyrtec are generally regarded to be compatible with breastfeeding again always double-check the active ingredients. The ingredients of claritine are safe while breastfeeding.
The principal symptom of lactose intolerance is an adverse reaction to products containing lactose primarily milk including abdominal bloating and cramps flatulence diarrhea nausea borborygmi and vomiting particularly in adolescents. Common signs and symptoms include.
 Signs Of Lactose Intolerance And What To Do Drformulas
Signs Of Lactose Intolerance And What To Do Drformulas
5 Awesome Shows Like Shark Tanks.
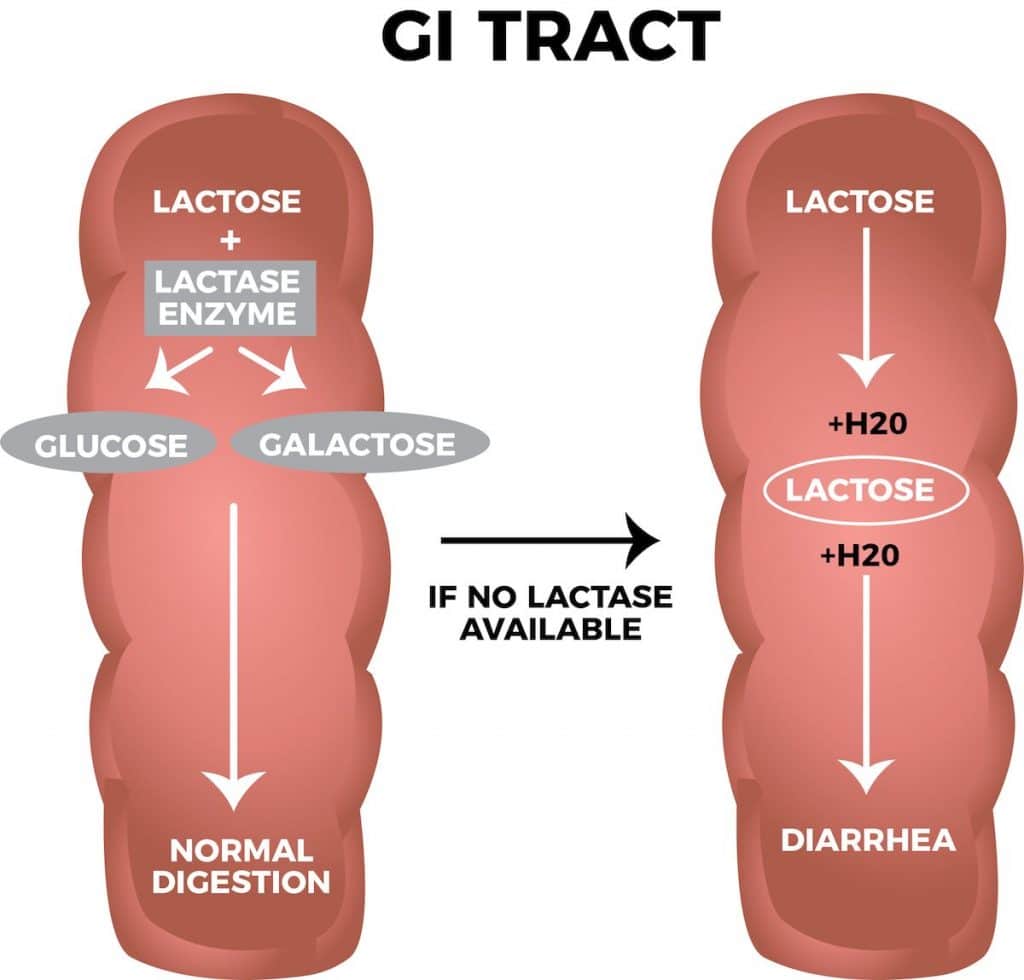
Symptoms of lactose intolerance. The signs and symptoms of lactose intolerance usually begin from 30 minutes to two hours after eating or drinking foods that contain lactose. Lactose intolerance is caused by a deficiency of the intestinal enzyme lactase that splits lactose into two smaller sugars glucose and galactose and allows lactose to be absorbed from the intestine. People with lactose intolerance may have a bloated stomach even though they do not overeat.
Lactose intolerance is very common affecting up to 70 of people worldwide. The symptoms of lactose intolerance described above can vary greatly from person to person. Lactose intolerance is the inability to digest lactose the sugar in milk and dairy products.
What are the symptoms of lactose intolerance. Symptoms of lactose intolerance usually develop within a few hours of consuming food or drink that contains lactose. Have you ever felt excessive flatulence bloating or even diarrhea after consuming milk.
Some people have pronounced complaints after every lactose-containing meal others feel little more than a slight discomfort. If you have lactose intolerance you may have symptoms within a few hours after you have milk or milk products or other foods that contain lactose. If youre always complaining of a stomach ache after enjoying a bowl of ice cream or noshing on a cheese board it could be because your stomach is not digesting lactose properly.
The most common symptoms include stomach pain bloating diarrhea constipation gas nausea and vomiting. These appear one-half to two hours after consumption. This test involves drinking half a glass of milk and seeing if symptoms develop.
Symptoms of lactose intolerance. When to see a doctor. Lactose intolerance is a common digestive problem where the body is unable to digest lactose a type of sugar mainly found in milk and dairy products.
Lactose intolerance is often inherited. Since bloating is also a bowel disease symptom consultation with a doctor is highly recommended. If you are lactose intolerant you will experience one or more of the following symptoms 30.
Primary lactase deficiency which is the most common type of lactose intoleranceIt is genetic and symptoms often appear when an infant. Nausea and sometimes vomiting. Lactose intolerance is a common digestive problem where the body is unable to digest lactose a type of sugar mainly found in milk and dairy products.
Make an appointment with your doctor if you frequently have symptoms of lactose intolerance after eating dairy foods particularly if youre worried about getting enough calcium. If yes then you are certainly lactose intolerant. If yes then you are certainly lactose intolerant.
Lactose intolerance is just one. Your symptoms may include. Vomiting sometimes Flatulence farting If you get these about 30 minutes to 2 hours after you drink milk or eat dairy products you should talk to your doctor.
Lactose intolerance is a digestive disorder caused by the inability to digest lactose the main carbohydrate in dairy products. Learn more about this common condition from WebMD. Secondary lactase deficiency.
Researchers have discovered that some people inherit genes from their parents that may cause a primary lactase deficiency. Love Watching Business Reality TV. Lactose intolerance is an inability to digest lactose the main sugar in milk which gives rise to gastrointestinal symptoms.
Stomach growling or rumbling sounds. Symptoms of lactose intolerance usually develop within a few hours of consuming food or drink that contains lactose. Degree of lactase deficiency.
The signs of lactose intolerance typically occur within 2 hours after consuming milk-based products. The following factors essentially influence the lactose intolerance symptoms. One of the most common signs that you have a lactose intolerance is abdominal pain or cramping that follows consumption of dairy products.
In addition to a swollen abdomen they may experience a sensation of fullness. Pain in your abdomen. Results from injury to the small intestine.
The main symptoms of lactose intolerance are abdominal discomfort or pain and watery diarrhea. A lactose challenge can help u determine whether a person is lactose intolerant or not. Symptoms of lactose intolerance until late adolescence or adulthood.
It can cause various symptoms including bloating diarrhea and.
A hard tender lump in one breast. Mastitis doesnt increase your risk of breast cancer.
 Mastitis Wise Specialist Emergency Clinic
Mastitis Wise Specialist Emergency Clinic
The symptoms of mastitis often appear suddenly and usually affect only one breast.

First signs of mastitis. This rare type of breast cancer causes breast skin changes. Mastitis is an inflammation of breast tissue thats common among breastfeeding moms. Symptoms typically include local pain and redness.
Some mothers who do not have any early signs of a blocked duct get mastitis out of the blue. Mastitis symptoms usually develop quickly and might include. Baby is less than 2 weeks old oryou have recently been in the hospital.
Flu-like symptoms such as fever fatigue and aches. It might feel hot and painful to touch a burning pain that might be continuous or happen while youre breastfeeding nipple discharge that is white or contains traces of blood. Warmth or redness of the overlying skin pain in the nipple area and.
You may begin to get shivers and aches. Mastitis is inflammation of the breast or udder usually associated with breastfeeding. Read on to know more.
But mastitis can occur in women who arent breast-feeding and in men. Mastitis is in both breasts. As a general guide.
Other common signs of infection include reduced milk production elevated body temperature lack of appetite and reduced mobility. Breast infection also termed mastitis is infection of the tissue in the breast in most individuals due to a bacterial infection. Signs of clinical mastitis in the udder are swelling heat hardness redness or pain.
Signs and symptoms of breast infections are redness of breast tissue pain and warmth of the breast body aches fatigue fever or chills and breast engorgement. These are the 10 most effective home remedies that worked for me. You might also have fever and chills.
Or you might wonder what mastitis looks like. The breast will be sore like it is with a blocked duct only worse. Some of the signs and symptoms of mastitis include.
Early symptoms of mastitis can make you feel as if you are getting the flu. These symptoms can include a wedge-shaped lump or hard patch in one of your breasts a red swollen area on the breast that may hurt. The affected breasts will often be reddened warmer than usual swollen and painful to the touch.
September 15 2018 Melanie 4 Comments. 10 Natural Home Remedies To Treat Mastitis That Work. Mastitis most commonly affects women who are breast-feeding lactation mastitis.
You may need to be evaluated in a hospitals emergency department if the breast pain is associated with other signs of an infection such as a fever swelling or redness to the breast and if. Mastitis is an inflammation of the breast occurring together with flu-like symptoms eg. Bloodpus is present in milk.
However mastitis symptoms are similar to inflammatory breast cancer symptoms. There is often an associated fever and general soreness. Signs may include dimples and a breast rash that has an orange-peel texture.
Mastitis usually only affects 1 breast and symptoms often come on quickly. It can either affect one breast or both. Complications can include abscess formation.
Onset is typically fairly rapid and usually occurs within the first few months of delivery. Usually only one breast is affected. In fact 1 in 10 moms may develop it while nursing.
It can happen any time during breastfeeding but usually occurs within the first 3 months after giving birth. Along with breast pain and warmth you may develop flu-like. Some individuals may develop tender somewhat mobile masses beneath the skin or deeper in the breast.
What are the first signs of mastitis. A swollen area on your breast that may feel hot and painful to touch the area may become red but this can be harder to see if you have darker skin. A red lump or area on the breast that is sore and hard.
First signs of mastitis. Burning sensation while breastfeeding lump inside the breast and redness on the breast are the first signs of mastitis. You may wonder what mastitis feels like compared to the normal tenderness you might feel when you first start breastfeeding.
Mastitis is an infection of breast tissue that most often occurs in women who breastfeed. You have broken skin on the nipplewith obvious signs of infection. Risk factors include poor latch cracked nipples use of a.
The inflammation results in breast pain swelling warmth and redness. Mastitis can be treated at home without antibiotics. Signs and Symptoms of Mastitis.
They will also sometimes have hardened lumps. Mastitis is most common in lactating women. Mastitis is an inflammation of the breast tissue most often caused by an infection.
Symptoms include a hard firm area in the breast that is usually painful. Mastitis is an inflammation of breast tissue that sometimes involves an infection.
Now youre doing a search for what cold medicine can you take while breastfeeding Luckily we are here to save you a little time. Also the benefit of continuing to take a medication for a chronic condition while breast-feeding often outweighs any potential risks.
.jpg) 12 Things No One Told You About Breastfeeding
12 Things No One Told You About Breastfeeding
Cold medicine and breastfeeding have to be considered with utmost care.

Cold medication while breastfeeding. The Drugs Listed Below are Usually Compatible with Breastfeeding Cold and Allergy Check for the word decongestant or the ingredient pseudoephedrine. Nasal sprays are generally considered compatible with breastfeeding. Adult Cold Flu Sore Throat is a drug containing multiple ingredients.
As a result its considered safe during breastfeedingand its often a go-to for controlling pain while recovering from childbirth injuries or C-sections. So here are your top 10 choices when you dont want to take meds. Simple diphenhydramine Benadryl and guaifenesin Robitussin are fine says Ross.
This information is not intended as a substitute for professional judgment. Often found in Alka Seltzer Plus Tylenol Cough Cold Vicks DayQuil and NyQuil and more Chlorpheniramine has been approved but large doses could also lower milk supply. Doxylamine succinate and diphenhydramine may cause sedation in mother and breastfeeding infant and should be used with caution if the infant has a history of apnea.
It might be better to start with these treatments because natural options are always healthier for the baby. Avoid the medications that have a multitude of active ingredients. If youre taking a medication that could be harmful to your baby your health care provider might recommend an alternative medication.
Safe Cold Medicines While Breast-Feeding Pseudoephedrine and phenylephedrine are oral decongestants for treating nasal congestion caused by colds allergies and sinus infections. Dextromethorphan has been studied in breastfeeding women and is considered safe. A new baby in the house can be exhausting.
Eye drops designed for coldallergy symptom relief are considered compatible with breastfeeding. Over-the-counter drugs containing dextromethorphan acetaminophen and ibuprofen are safe to take while breastfeeding. Phenylephrine is likely that it is safe while breastfeeding.
You should choose a cold medication that contains only one safe ingredient to effectively treat your primary symptom. Still a few medications arent safe to take while breast-feeding. Simple diphenhydramine Benadryl and guaifenesin Robitussin are safe to take while.
Decongestant nasal sprays are generally for short-term use 3-7 days only. Zinc Gluconate is considered safe for breastfeeding moms and their babies. If you need an antihistamine also used to treat allergies they are generally considered safe.
Please check each of the links below where breastfeeding lactation information is available. Other Remedies for Cold While Breastfeeding. Unsafe cold meds while breastfeeding.
Medicines with the active compound acetaminophen like Tylenol Crocin etc can be taken for a cold while breastfeeding. These medications help with pain that may come with a cold like headaches muscle aches or a sore throat. Always consult your physician.
Be careful about taking Tylenol while youre also taking cold and flu products like Nyquil DayQuil Excedrin or Robitussin though. There are several at-home cold remedies for breastfeeding women you just need to know where to find them. Besides cold medicine breastfeeding mothers can use there are also some alternative remedies to try.
Rub mentholated cream on your chest and under your nose. Zinc works by stopping the rhinovirus from multiplying. Consult your health care provider and the package instructions for specific information.
Ibuprofen Advil Motrin and acetaminophen Tylenol are usually considered safe to take while breastfeeding. Zinc gluconate is a commonly recommended cold remedy considered safe to use while breastfeeding. Work with your doctor to find a medication that treats your condition and is safe while breastfeeding.
The cough suppressant dextromethorphan has long been used during breastfeeding and is considered safe. You might find them alone but youll also notice them combined with other cold medications. Yes with some exceptions.
An analgesic acetaminophen can relieve you from fever inflammation and pain. But when you add any kind of illness even a cold on top of that it can flat out drain you. Often found in Coricidin and more.
The nasal gel preparation is recommended over oral drops. Following are the cold medicines that you should definitely avoid when breastfeeding. What cold medicine can you take while breastfeeding.
Zinc is a mineral that is essential for cellular enzymatic. Adult Cold Flu Sore Throat use while Breastfeeding. Cold Medications That are Safe to Take While Breastfeeding.
And you can take ibuprofen Motrin Advil and aspirin while breastfeeding which were a no-no for pregnant. Nasal sprays or gels. Can I take medications and breastfeed.
In many cases zinc has been shown to reduce the duration of a cold by up to a day especially when taken within the first 24 hours of symptoms starting.

:max_bytes(150000):strip_icc()/how-to-get-pregnant-faster-1960275_V2-01-7d9b54056604480e9f9647d026f32972.png)